March 5, 2015
The 1918 Flu Pandemic: A Look Back on One of the Deadliest Natural Disasters in Human History
By Terry Masek, SPHR
Human Resources Officer
Metropolitan Medical Laboratory, PLC
World War I claimed an estimated 16 million lives. The influenza epidemic that swept the world in 1918 killed an
estimated 50 million people. It has been cited as the most devastating epidemic in recorded world history. One-fifth of the world’s population and one-quarter of the United States were attacked by this deadly virus. Within months, it had killed more people than any other illness known to man.
For decades, scientists have debated where in the world the pandemic started, variously pinpointing its origins in France, China, the American Midwest and beyond. Without a clear location, scientists have lacked a complete picture of the conditions that bred the disease and the factors that might lead to similar outbreaks in the future.
The Beginning
The plague emerged in two phases. In late spring of 1918, the first phase, known as the “three day fever,” appeared without warning. Few deaths were reported and victims recovered after a few days. But in August of 1918, when the second wave began, the virus had mutated into a much deadlier form. Some of the developments that helped to set the stage for the dark days to come have been attributed to the circumstances of World War I.
In civilian life, natural selection favors a mild strain. Those who got very ill stayed home, and the mildly ill individuals continued with their lives, preferentially spreading the mild strain. In the trenches of war in 1918, natural selection was reversed. Soldiers with a mild strain stayed where they were, while the severely ill were sent on crowded trains to crowded field hospitals, spreading the deadlier virus. The second wave of this plague began, and a stronger version of the flu quickly spread around the world again.
Of the U.S. soldiers who died in Europe during World War I, half of them fell to the influenza virus and not to the enemy. In order to maintain morale during World War I, wartime censors minimized the early reports of illness and mortality in Germany, Britain, France and the United States, but newspapers were free to report the epidemic’s effects in neutral Spain, where 8 million people died, thus helping to give the pandemic the nickname Spanish Flu. The influenza pandemic circled the globe. It spread, following the path of its human carriers, along trade routes and shipping lines.
A Strong and Deadly Strain
Most influenza outbreaks disproportionately kill young, elderly or already weakened patients. In contrast, the 1918 pandemic predominately killed previously healthy young adults by causing a “cytokine storm,” which is an overreaction of the body’s immune system. The strong immune reactions of young adults ravaged their bodies, whereas the weaker immune systems of children and middle-aged adults resulted in fewer deaths among those groups.
The most vulnerable of all – those most likely to die – were pregnant women. In studies of hospitalized women in the pandemic, the death rate ranged from 23 percent to 71 percent. Of the pregnant women who survived childbirth, over one-quarter (26 percent) lost the child. Symptoms in 1918 were so unusual that initially influenza was misdiagnosed as dengue, cholera or typhoid. The majority of deaths were from bacterial pneumonia, a secondary infection caused by influenza, but the virus also killed people directly, causing massive hemorrhages and edema in the lung. This unusually severe disease killed up to 20 percent of those infected, as opposed to the usual flu epidemic mortality rate of 0.1 percent.
Life in America a Century Ago
During the early twentieth century, communicable
diseases – that is diseases which can spread from person to person – were widespread. Influenza and pneumonia along with tuberculosis and gastrointestinal infections such as diarrhea killed Americans at an alarming rate, but non-communicable diseases such as cancer and heart disease also exacted a heavy toll. Accidents, especially in the nation’s unregulated factories and workshops, were also responsible for maiming and killing many workers.
High infant mortality also shortened life expectancy. In 1918, one in five American children did not live beyond their fifth birthday. In some cities, the situation was even worse, with 30 percent of all infants dying before their first birthday. Childhood diseases such as diphtheria, measles, scarlet fever and whooping cough contributed significantly to these high death rates.
Life expectancy in the United States today is 81 years for a woman and 76 years for a man. In 1918, life expectancy was 54 years for women and 53 years for men. Due to the impact of the influenza epidemic, the average life expectancy in this country dropped by 10-12 years.
A Killer Stalks the World
The disease killed in every corner of the globe. As many as 17 million died in India, about 5 percent of the population. In Tahiti, 13 percent of the population died during a single month. Similarly, in Samoa, 22 percent of the population of 38,000 died within two months. In Ghana, the epidemic killed at least 100,000. In Brazil, 300,000 died, including their president. In Britain 250,000 died. In France, more than 400,000. In the US, approximately 28% of the population suffered and 675,000 people died out of a total population of 105 million. The numbers were approximations because, in 1918, the Public Health Service didn’t recognize influenza as a reportable disease.
In October of 1918, Congress appropriated a million dollars for the Public Health Service to recruit and pay for additional doctors and nurses. The existing shortage of doctors and nurses, caused by the war, made it difficult to locate and hire qualified medical professionals. The virulence of the disease also meant that many doctors and nurses contracted influenza within days of being hired.
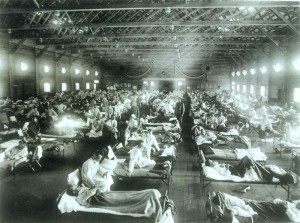
Confronted with a shortage of hospital beds, many local officials ordered that community centers and local schools be transformed into emergency hospitals. In some areas, the lack of doctors meant that nursing and medical students were drafted to staff these makeshift hospitals. In Chicago at the height of the epidemic, physicians were seeing sixty to ninety patients a day, unable to do much besides trying to make them comfortable.
As the disease spread in the U.S., schools and businesses emptied. Telegraph and telephone services collapsed as operators took to their beds. Garbage went uncollected as sanitation workers reported sick. The mail piled up as postal carriers failed to come to work.
State and local departments of health also suffered from high absenteeism rates. The Public Health Service’s requests for information went unanswered.
As the bodies of the dead accumulated, funeral parlors ran out of caskets and bodies went uncollected in morgues. Besides the lack of health care workers and medical supplies, there was also a shortage of coffins, morticians and gravediggers. Mass graves were dug by steam shovel and bodies were buried without coffins in many places.Quarantines were imposed to prevent the spread of the disease. Schools, theatres, saloons, pool halls and even churches were all closed. As bodies mounted, even funerals were held outdoors to protect mourners against the spread of the disease.
One recollection shared from 1918 told the story of four women playing bridge together late into the evening. Overnight, three of the women died from influenza. Others told stories of people on their way to work suddenly developing the flu and dying within hours.
In a local connection, Dr. Frederick Lamb, the first pathologist in the Quad Cities, was a captain in the U.S. Army Medical Corps, stationed as Chief of Laboratory Service at Camp Cody, New Mexico in 1918. He co-authored a paper in The Journal of the American Medical Association (April 12, 1919, pages 1056-62) describing the onset and effects of the influenza epidemic in the autumn of 1918. On October 21, 1918, the first batch of 5000 draftees arrived at Camp Cody for training. On October 26 alone, 378 patients were admitted to the hospital with influenza. Dr. Lamb stated that their hospital, 1200 beds in normal times, held 2153 patients on October 30, 1918. Of the hospitalized patients that day, 1899 had influenza or pneumonia. Deaths among the previously healthy – mostly young – soldiers with influenza were 7.3% overall and 38.4% in those with pneumonia. During the epidemic, 75 of their 100 nurses contracted influenza and 5 died from it.The JAMA paper lists some of the measures taken to try to slow the spread of the causative organism, which was spread by air-borne respiratory droplets (although physicians didn’t know it was a virus yet) and reports some additional observations on the course of the disease in October and November of 1918.
The virus killed 200,000 in the U.S. in October of 1918 alone. On November 11, 1918 there were mass celebrations on Armistice Day to observe the end of World War I, but that close-contact behavior led to more exposure and a rebirth of the epidemic in some cities.
Hundreds of thousands of Americans who survived the disease were orphaned and widowed.
Science to the Rescue
In the nineteenth century, most physicians and public health experts believed that disease was caused not by microorganisms but rather by dirt itself. As science evolved and physicians became more enlightened, it became apparent that access to clean water and the availability of better sewage systems would have a positive impact on the overall health of the population. By 1918, improved water and sewage systems had greatly contributed to a decline in gastrointestinal infections and a significant reduction in mortality rates among infants, children and young adults.
Educational campaigns to emphasize personal hygiene and community health were crucial steps in the battle against disease, but, because many Americans were illiterate or were not fluent in English, these campaigns had to rely heavily on the use of images to convey their message.
As Americans’ understanding of disease evolved and as physicians and laypeople came to understand that microorganisms – or germs – caused diseases, public health campaigns became more sophisticated. These newer campaigns continued to advocate cleanliness as a means of preventing disease, but they also urged people to avoid germs, the causative agent of disease.
After the lethal second wave of this flu struck in late 1918, new cases dropped abruptly – almost to nothing after the peak of the second wave. One explanation for the rapid decline of the lethality of the disease is that doctors simply got better at preventing and treating the pneumonia that developed after the victims had contracted the virus. Another theory holds that the 1918 virus mutated extremely rapidly to a less lethal strain.
The Legacy of the 1918 Pandemic
The 1918 flu has been described as “the greatest medical holocaust in history” and may have killed more people than the Black Death, a pandemic that devastated Europe from 1346 to 1353 and wiped out an estimated 60% of the population there. The 1918 virus was responsible for 25 million deaths in the first 25 weeks of the pandemic. No other illness has ever harmed so many over such a short period of time. It is said that this flu killed more people in those 25 weeks than AIDS has killed in 25 years – and more in a year than the Black Death killed in a century.
Today, we’re acutely aware of new diseases like Ebola, dengue fever, avian influenza, the West Nile virus and various mutations of hemorrhagic fever conditions around the world. Unfortunately, this list will only grow as medical science works to understand these new diseases – and ultimately to develop immunizations to protect us from them. It’s a never-ending battle with potentially cataclysmic consequences. Even with modern antiviral and antibacterial drugs, vaccines and prevention knowledge, the return of a pandemic virus equivalent in pathogenicity to the virus of 1918 would likely kill more than 100 million people worldwide.
Let’s hope that science has the knowledge and the ability to stay ahead of such a doomsday scenario.
Metropolitan Medical Laboratory has recently celebrated our 100th year of service to the Quad City community. Your good health continues to be our passion. Metropolitan Medical Laboratory, PLC is one of the largest accredited laboratories in the states of Illinois and Iowa. Visit www.metromedlab.com. Tell your doctor, “I want to go to Metro.”
Your good health continues to be our passion. Metropolitan Medical Laboratory, PLC, is one of the largest accredited laboratories in the states of Illinois and Iowa, and has provided this community with quality laboratory services for the past 100 years. Next time you need lab work done, tell your doctor, “I want to go to Metro.”
Filed Under: History
Trackback URL: https://www.50pluslife.com/2015/03/05/the-1918-flu-pandemic-a-look-back-on-one-of-the-deadliest-natural-disasters-in-human-history/trackback/